Nothing Butt the Truth: Understanding Anal Cancer

CRACKING THE CODE: ANAL HEALTH 101
Today is World Cancer Day, and in observance of that we wanted to take a minute to educate you on one type of cancer that doesn’t get enough attention: anal cancer. Yup, butts. We’re talking about butts.
I’ll say that in med school, anal health wasn’t a focus; it was just about prostate exams. We all gathered round and got to feel a prostate; that was that. After becoming a doctor and spending years in primary care, I shifted my focus to LGBTQ+ health at Rush University Medical Center, leading the charge in that area. A physician I had referred many anal health patients to asked me to join his practice, and at first I was like, “I don’t want to do that. That’s why I refer it out.” But eventually, with everything going on in medicine and everything I had seen, I said, “Let’s give this a shot.” I ended up here by recognizing the demand for LGBTQ+ health and following where it led me.
Surprisingly, anal health lacks a defined medical focus, and the field has limited standardized education. It’s not a specialty like cardiology. However, at Howard Brown Health, it’s a crucial department due to our community’s specific needs. While various medical professionals practice anal health in different capacities, Howard Brown’s unique focus demands a specialized program, which is something I’m genuinely proud to run.
“Howard Brown’s unique focus demands a specialized program, which is something I’m genuinely proud to run.”
Dr. Gregory rauch
In anal health, our main emphasis is on screening and preventing anal cancer, particularly among people engaging in anal sex, especially men who have sex with men. The main thing that I run into are symptoms like bleeding, itching, or lumps, though those don’t necessarily indicate anal cancer. While I certainly understand that discussing this topic can be uncomfortable, at Howard Brown we recognize and navigate our community’s sensitivities while still providing the vital care they need. I have patients who have experienced trauma related to that area and need careful consideration, but I also have patients who will joke around and make sex jokes during procedures. So, it can really go both ways.
We also know that outside of Howard Brown, patients may encounter obstacles like discrimination or discomfort when discussing anal health. To mitigate harm, we aim to refer patients within our organization to experienced, affirming providers.
“It’s important that we break down these social barriers to accessing care so that we can prioritize our community’s health.”
Dr. Gregory Rauch
The primary challenge that I see with patients is their reluctance to discuss these matters, often due to embarrassment. Which… I get. Butts are awkward and most of the time we don’t show them to people we just met. But it’s important that we break down these social barriers to accessing care so that we can prioritize our community’s health.
When it comes to your butt – regardless of sexual orientation – engaging in anal activities can strain the body. Being mindful of what’s normal or not is crucial for cancer screening and overall health. In essence, the more you use your butt, the more attention it deserves for maintaining good health. So, make sure you know what’s going on down there: a small mirror, your camera phone, or a partner can all help you keep tabs on what your body looks like.
We have been testing and evolving our anal health screening guidelines here at Howard Brown and we are unique in providing procedural guidance for all our doctors. Our organization-wide awareness ensures that all providers can refer patients appropriately and conduct screenings themselves. In many other organizations, screenings are lacking and anal health specialists are rare. Patients are often referred to colorectal surgeons for this care, but they tend to focus more on surgery than discussing issues like pain or difficulty with sex.
Here at Howard Brown Health, we want to know if bottoming is going well for you or not. We’ll recommend some toys to try or ways you can reduce discomfort, too. We’re not squeamish. So let’s get into some specifics.
BOOTY BASICS
Avoid Wet Wipes
One major concern for anal health is the use of wet wipes. Contrary to common belief, frequent use of wet wipes often exacerbates issues, causing irritation and complications. While using them occasionally might not cause issues, regular use tends to worsen existing problems. I’d recommend a bidet for a quick clean that won’t irritate you.
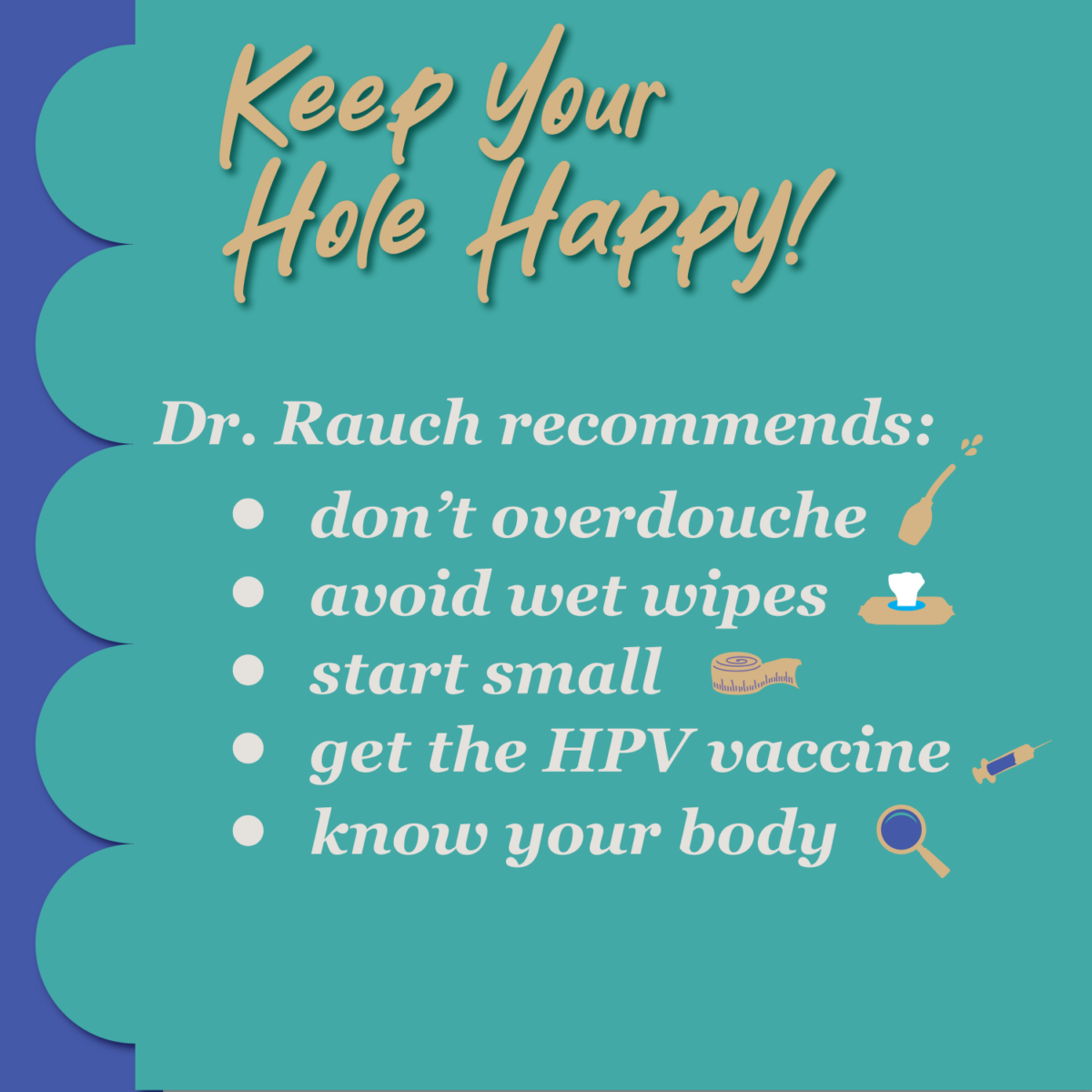
Start Small
When it comes to engaging in anal activities, I encourage exploration but emphasize the importance of proceeding thoughtfully. Gradual progression is key, especially for those who may have been inactive for a while. Rushing into substantial activities can lead to fissures and complications, requiring downtime before returning to such activities. You can’t become a size queen overnight.
Soothe Irritation
For managing irritation, I recommend Balneol, which you can find at drug stores or online. It’s effective, and you can even find it in wipe form. If issues persist, seeking professional advice is crucial to rule out any underlying problems.
Avoid Straining
When it comes to bowel movements, prioritize avoiding straining. We all love to sit down and scroll TikTok on the toilet, but avoid sitting for too long. It’s essential not to spend excessive time on the toilet, as it worsens conditions like hemorrhoids. Increasing fiber intake and staying hydrated are more effective than relying solely on tools like squatty potties.
Don’t Overdo(uche) It
When douching, gentleness is key, especially with firm-tipped devices to prevent scratches. Shower shots and the like are convenient, but your anus doesn’t need power washing. Only douche when necessary, avoiding unnecessary or excessive pressure. Constant douching isn’t natural for our bodies. With the advent of cruising apps, some people may feel the need to be “ready to go” at all times, even at the grocery store. Don’t. It’s easy to pour your friend a drink and hit the bathroom quickly before anything happens. Over-douching and practices like that can contribute to irritation and the risk of conditions like anal cancer.
BUTT OUT, CANCER!
Which brings us to the final and maybe most important point of this post. Anal cancer.
Anal cancer is relatively rare, but certain factors increase the risk. Living with HIV, regardless of undetectable levels, is a significant risk factor. Because of this, Howard Brown Health has dedicated time and resources to making sure we are screening our patients for anal cancer. Additionally, high-risk strains of the Human Papilloma Virus (HPV), especially type 16, are linked to anal cancer. Other minor risk factors include tobacco use, a history of anal or genital warts, and low T cell counts (for those with HIV). For a comprehensive list of screening guidelines published this week by IANS, check out this article.

HPV itself is widespread and while there are over a hundred types, only a subset is associated with anal cancer. The link between HIV and anal cancer is thought to be related to a compromised immune system, but clinical research is still trying to fully understand the connection, as even those with undetectable viral loads remain at a higher risk.
Even if you’re living with HIV but not regularly engaging in receptive anal sex, it remains a risk factor. Risk is higher if you’ve had anal sex, and while not engaging in it lowers the risk, it’s still increased with HIV. Taking PrEP is crucial.
For screening anal cancer, those at risk or engaging in receptive anal sex should be vigilant for symptoms like unusual pain, bleeding, or lumps. Self-swabs are less effective, so it’s recommended to have a primary care doctor perform a quick 20-second swab. Unfortunately, screening may sometimes be overlooked by primary care providers and these concerns can be awkward to bring up. At Howard Brown, my goal is to ensure everyone with risk factors gets screened.

Since most cancers show no symptoms, treating any detected symptoms is recommended, as determining the dangerous ones is challenging. One of the best tools for identifying issues is a high-resolution anoscope (HRA). A high-resolution anoscopy involves using a microscope to examine the anus for abnormalities. Typically, individuals first undergo an initial PAP high-risk HPV test. If results show abnormalities, I perform the high-resolution anoscopy. It includes numbing gel, vinegar to highlight HPV-damaged areas, iodine application, and biopsy for abnormalities, usually painless.
For those with HIV, regular screenings are recommended at ages 35 and up. For others with risk factors, screenings are recommended around age 45, following new guidelines. These are flexible and symptomatic cases may require earlier screening. People with a history of receptive anal sex should discuss this with their primary care provider. If you’re around 25, focus on getting the HPV vaccine for reduced risk. Gardasil is the most common HPV vaccine and while it is primarily used to prevent cervical cancer, its role in preventing anal cancer is gaining recognition.
My hope is to raise awareness about anal cancer and ensure those who need screening receive it. It’s crucial for everyone to have access to high-quality care to prevent unnecessary loss of lives. Education is key, especially for those in smaller towns without easy access to specialized healthcare. Providing data and referring to reputable sources like The Anchor Study and The International Anal Neoplasia Society can help individuals advocate for themselves.
“My hope is to raise awareness about anal cancer and ensure those who need screening receive it.”
Dr. gregory rauch
In the fight against misinformation, prejudice, and stigma, education and evidence play vital roles. The bottom line: everyone has a butt and it’s okay to discuss any issues you’re having with it. On World Cancer Day, prioritize your well-being, get screened if necessary, and join us in spreading awareness about anal cancer. Stay healthy!

